Focusing on blood biomarkers changes the way we think about timing and intervention. If metabolic health shifts the biological clock for neurodegeneration, then weight, inflammation, and related metabolic factors become urgent targets for prevention strategies. Clinicians, caregivers, and people at risk need tools that reveal risk sooner so lifestyle changes, medications, or tailored supports can be tried while there is still time to influence outcomes.

The study raises practical and ethical questions about screening, access, and how societies support healthy aging. Learning that obesity speeds detectable Alzheimer’s processes presses us to design inclusive programs that reduce barriers to preventive care. Click through to see how the authors link blood-based signals to brain imaging and consider what that means for expanding early detection and equitable approaches to protecting cognitive health.
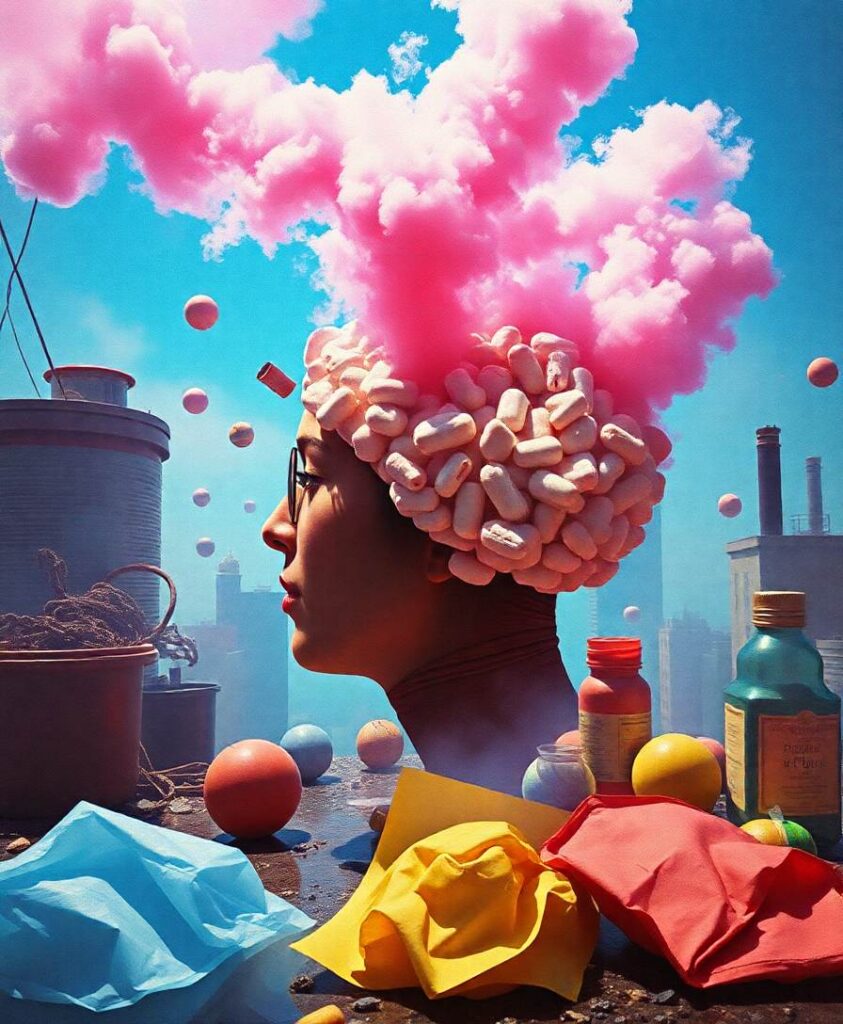
Obesity accelerates the rise of Alzheimer’s-related blood biomarkers far more rapidly than previously recognized. Long-term imaging and plasma data show that obese individuals experience much faster increases in proteins linked to neurodegeneration and amyloid buildup. Surprisingly, blood tests detected these changes earlier than PET scans. The results point to obesity as a major, modifiable contributor to Alzheimer’s progression.