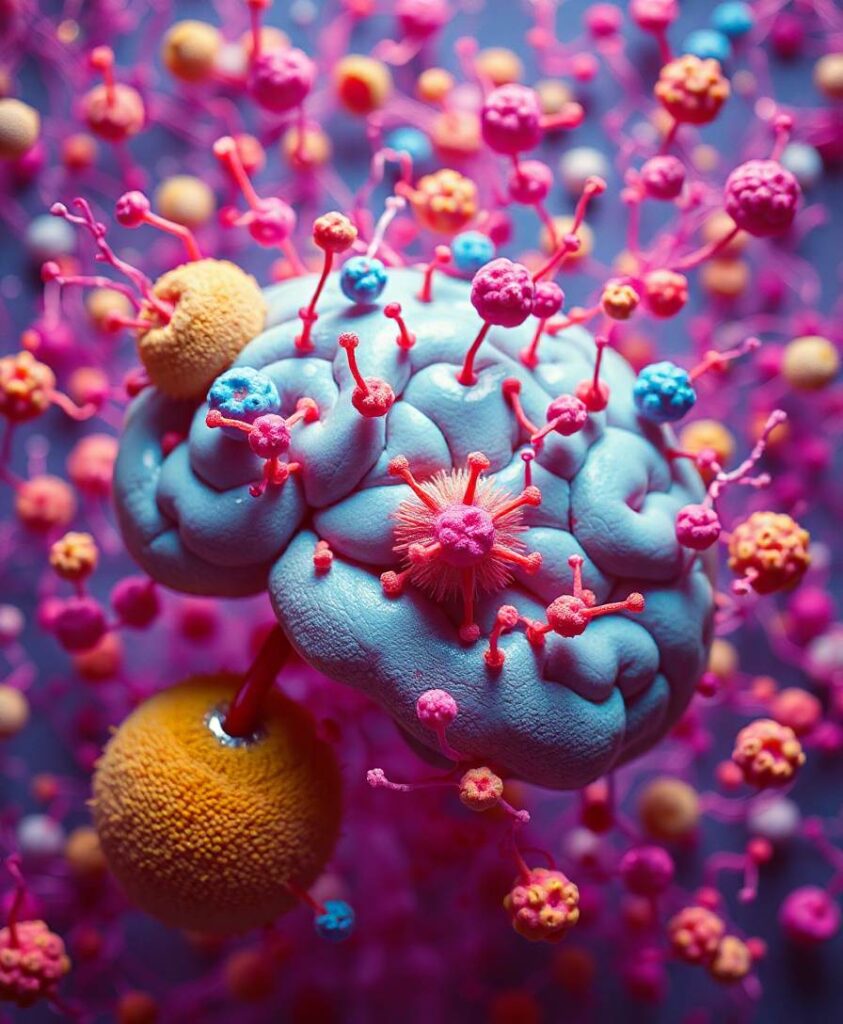
A regular sleep-wake cycle plays a positive function that preserves synaptic plasticity and brain activity from neuropathological injuries. The hypothalamic neuropeptide orexin-A (OX-A) is central in sleep-wake regulation and has been found to be over-expressed in the cerebrospinal fluid (CSF) of patients with Alzheimer’s disease (AD) suffering from sleep disturbances. OX-A promotes the biosynthesis of 2-arachidonoylglycerol (2-AG), which, in turn, could be phosphorylated to 2-arachidonoyl lysophosphatidic acid (2-AGP). The reorganization of the actin cytoskeleton during neurite retraction is one of the best-characterized effects of lysophosphatidic acids. However, less information is available regarding the reorganization of the neuronal microtubule network in response to OX-A-induced 2-AG and, possibly consequent, 2-AGP production in AD patients. This is of special relevance also considering that higher 2-AG levels are reported in the CSF of AD patients. Here, we found a positive correlation between OX-A and 2-AGP concentrations in the plasma, and an increase of 2-AGP levels in the CSF of AD patients. Furthermore, a negative correlation between the plasmatic 2-AGP levels and the mini-mental state examination score is also revealed in AD patients. By moving from the human patients to in vitro and in vivo models of AD we investigated the molecular pathway linking OX-A, 2-AG and 2-AGP to the phosphorylation of pT231-Tau, which is a specific early plasma biomarker of this disorder. By LC-MS analysis we show that OX-A, via OX-1R, induces 2-AG biosynthesis via DAGLα, and in turn 2-AG is converted to 2-AGP in primary hippocampal neurons. By confocal microscopy and western blotting assay we found an OX-A- or 2-AGP-mediated phosphorylation of Tau at threonine 231 residue, in a manner prevented by LPA1R (2-AGP receptor) or OX1R (OX-A receptor) antagonism with AM095 or SB334867, respectively. Finally, by patch-clamp recording we documented that 2-AGP-mediated pT231-Tau phosphorylation impairs glutamatergic transmission in the mouse hippocampus. Although further additional research is still required to clarify the potential role of orexin signaling in neurodegeneration, this study provides evidence that counteraction of aberrant OX-A signaling, also via LPA-1R antagonism, may be beneficial in the mild-to-moderate age-related cognitive decline associated with sleep disturbances.