The Post-amyloid Era in Alzheimer’s Disease: Trust Your Gut Feeling
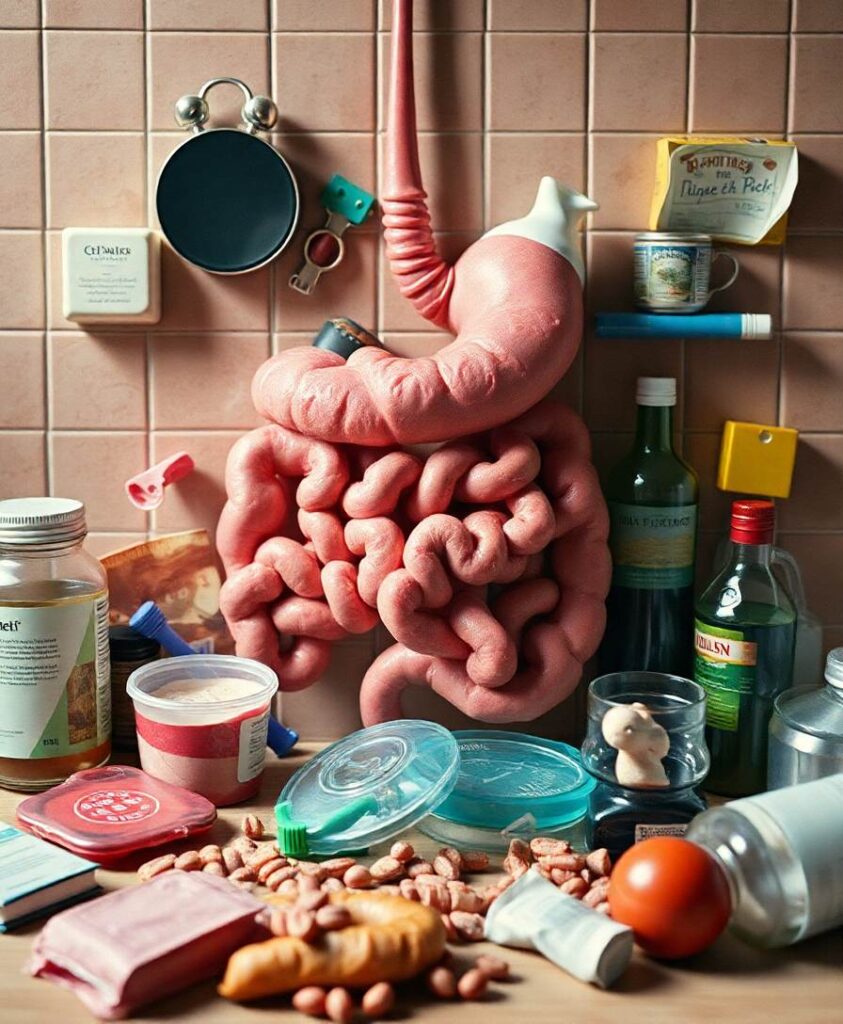
Amyloid hypothesis, the assumption that beta-amyloid toxicity is the primary cause of neuronal and synaptic loss, has been the mainstream research concept in Alzheimer’s disease for the past two decades. Currently, this model is quietly being replaced by a more holistic, “systemic disease” paradigm which, like the aging process, affects multiple body tissues and organs, including the gut microbiota.
It is well-established that inflammation is a hallmark of cellular senescence, however the infection-senescence link has been less explored. Microbiota-induced senescence is a gradually emerging concept promoted by the discovery of pathogens and their products in Alzheimer’s disease brains associated with senescent neurons, glia and endothelial cells.
Infectious agents have previously been associated with Alzheimer’s disease, but the cause vs. effect issue could not be established. A recent study may have settled this debate as it shows that gingipain, a Porphyromonas gingivalis toxin, can be detected not only in Alzheimer’s disease but also in the brains of older individuals deceased prior to developing the illness.
In this review we take the position that gut microbes and their molecules reach the brain by triggering intestinal and blood brain barrier senescence and disruption. We also surmise that novel Alzheimer’s disease findings, including neuronal somatic mosaicism, iron dyshomeostasis, aggressive glial phenotypes and loss of aerobic glycolysis can be explained by the infection-senescence model. In addition, we discuss potential cellular senescence targets and therapeutic strategies, including iron chelators, inflammasome inhibitors, senolytic antibiotics, mitophagy and epigenetic metabolic reprograming.
Amir is a Pakistani-Canadian neuroengineer in Toronto, developing brain-computer interfaces to enhance learning. As a volunteer author, he shares insights on how technology can amplify cognitive abilities, drawing from his diverse South Asian-Canadian perspective.